Visceral fat is a dangerous herald of health problems. The worst thing is that it is invisible to the eye, and there are simply no clear characteristics of its redundancy for determining “by eye”.
The harm of visceral fat and its effect on the functioning of internal organs
Visceral fat is a layer of fat cells around vital organs: the heart, liver, gastrointestinal tract, kidneys, etc., located in the chest cavity, pelvis and abdomen. It also occurs in incomplete people, so normal weight indicators are not a guarantee of the absence of visceral fat. In addition, its dosed presence is the norm for each person, providing depreciation of organs.
Balanced is the presence of a visceral layer within 10-15% of the total fat mass. Anything above these figures is redundant.
According to a study by American scientists, a large amount of visceral fat leads to the following diseases:
- type II diabetes;
- work disruption of cardio-vascular system;
- cancerous tumors and pathological neoplasms;
- dementia;
- respiratory diseases;
- hormonal disruptions;
- metabolic disorders.
Scientists note that visceral obesity has become particularly relevant in recent years. And the most common topic is the accumulation of fat around the heart muscle. Since it is difficult to deal with it, and surgical intervention to eliminate this problem is unacceptable, society is in dire need of innovative methods for treating this disorder.

Visceral obesity in men and women
The fact that the female half of society has more fat is well known. But this malicious pest of slender forms is deposited in lovely ladies mainly in the subcutaneous areas of problem areas: on the abdomen, hips, buttocks. Estrogen helps them fight it. As for men, they tend to accumulate visceral fat at a rapid pace. It is formed in them faster than usual, however, and goes away when losing weight in the first place.
An illustrative example is when a man gains weight, slightly increasing volumes in the waist area. The fact is that it is visceral fat that plays a role in increasing the readings of the scales. When losing weight, first there is a drop in weight, and then body volumes. So the body feeds itself with energy, first visceral, and then subcutaneous fat.

Visceral fat deposits - where do they come from
The omentum is often the site of visceral fat deposition. This leads to the growth of the abdomen. At the same time, the legs can remain slender. This type of obesity is characteristic mainly for those who are often under the influence of stress. Even the notorious "beer belly" is also a herald of the growth of body fat around the internal organs.

Accurate data on an excess of visceral fat in the body can only be given by a doctor with the appropriate qualification in MRI or tomography, everything else is an approximate definition. However, it can also cause a change in the wrong lifestyle. Either way, it's good for your health. If you do not have a special device "Tanita", with which representatives of the company used to go proper nutrition and fat-burning drinks, just measure your waist. In women, it should normally not exceed 89 cm (35 inches), while in men it can be up to 98 cm (40 inches).
For a more accurate home measurement, the definition of the coefficient is suitable. To do this, you need to divide the waist circumference by the hip circumference. The female version of the norm does not step over 0.88, in men it does not exceed 0.95. Everything that is above the upper limit is an excess of visceral fat, which must be fought.
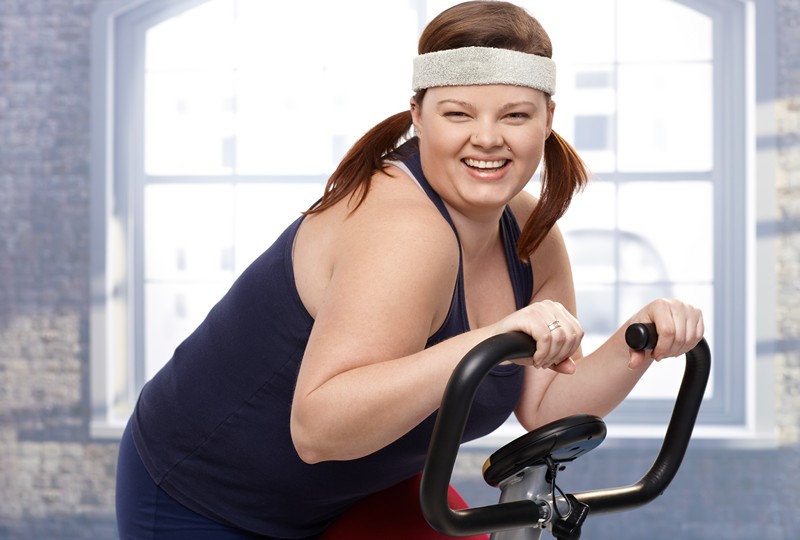
For women, types of a safe figure with thin waist are "pear", "guitar" and "hourglass". But visceral fat can be found in excess even in slender people. This phenomenon is partly explained by genetics and the "inheritance" inherited from the parents, but to a greater extent, this is due to the lack of proper physical activity. British doctors say that by maintaining a figure only with diets and without resorting to exercise complexes, we can thereby increase visceral fat. Therefore, you should not limit yourself to waist measurements. Add activity to your life: walk, run in the morning, pump the press and dance in training. All this will give good results.

No matter how trite it may sound, the recommendations of nutritionists and people who are passionate about a healthy lifestyle will help get rid of visceral fat.
Visceral Fat Loss Program:
- Nutrition Switching to a rational diet will give a good result. Ideally, if the nutrition system is developed by a specialist who knows your parameters and the results of blood tests. But if you don’t feel like going to the hospital, you can independently limit yourself from fatty, starchy, sweet, salty and spicy foods. Preferably steam or boil foods. Grilling without oil and baking “on tracing paper” will do. The diet should be based on healthy foods: cereals, vegetables, fruits, whole wheat bread fish, lean meats, etc.
- Physical exercise Going to the gym on strictly allotted days will keep your body in good shape and will be addictive, which means that over time you will enjoy training. Moreover, there you are not in splendid isolation, and other people's successes always stimulate. But if you do not allow laziness to overcome yourself, you can study at home. To do this, you can turn on the video program and repeat the complexes shown in it, you can print the diagram on the Internet and strictly follow the instructions, you can remember the effective exercises of your student or school years. The main thing is to work out all the muscles of the body, not to be lazy to do several approaches in the same exercise. Your body will begin to expend internal energy, eating fat reserves.
- Lifestyle and bad habits It is necessary to give up alcohol, smoking, visiting fast foods, even on weekends. Such pampering is usually expensive. It is very important to develop correct mode, and in everything. Try to have breakfast-lunch-dinner around the same time, accustoming yourself to a healthy schedule. Go to bed at least two hours before midnight, get enough sleep, but you can get up with the first roosters. During the day, especially if you have a sedentary job, try to take small breaks for rest, light warm-up of the muscles of the body.
Detailed video about visceral fat
Of course, starting to follow these rules at once is difficult. The rhythm developed over the years changes with difficulty. But if your goal is to improve the body and get rid of visceral fat, then gradually begin to form a new lifestyle. It is he who will allow you not to suffer from ailments acquired through your own fault.
In most cases, the motivation to lose weight is associated with the desire to simply look better, but obesity is not only ugly folds on the sides and three chins, but also a direct threat to health.
Types of obesity, or what is visceral fat
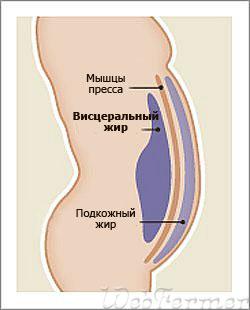
Visually, we immediately notice excess under the skin, the so-called subcutaneous fat, but there are adipocytes throughout the body, and of course, with excess weight, fat deposits accumulate in body cavities too.
Around all internal organs there is always a small fatty layer inside the so-called visceral membranes. In the abdominal cavity it is the peritoneum, around the heart - the pericardium, around the lungs - the pleura. The fat cells located here are able to accumulate fat in the same way as subcutaneous ones, but the harm from visceral obesity is much greater.
Visceral obesity also called abdominal, since fat deposition occurs in body cavities, especially in the abdominal cavity. Even the heart can become fat.
Why is visceral fat dangerous?
In a healthy person, visceral fat helps the organs stay in place, protects them from injury and cold, but if its amount is excessive, this is a threat to health.
Visceral obesity is directly related to the risk of developing metabolic syndrome(this is a deadly quartet of 4 diseases: type 2 diabetes, hypertension, coronary heart disease and obesity).
Subcutaneous fat is less dangerous, but if you have a significant body mass, the internal organs will still suffer to some extent.
Visceral obesity in men and women
The deposition of fat around the internal organs is imperceptible, unlike the subcutaneous fat layer. This type of obesity is called androgynous, since such fat deposition is most typical for men.
Among women high level hormones - estrogen causes the predominant deposition of fat in the thighs and buttocks, in the lower abdomen. So it is necessary for the successful bearing of offspring. Of course, the increase in volumes for women will be obvious. In men, overnutrition does not affect the health for a long time. appearance while body weight is increasing. The body stores all its reserves in internal organs and it's not that noticeable.
Starting to lose weight, women quickly lose in volume and in parallel in weight, while with visceral obesity, volumes do not disappear at first glance, despite the weight loss. And only with significant weight loss there comes a moment when the stomach also loses weight.
External manifestations of visceral fat are visible in people with hormonal disorders, in beer drinkers and men living in conditions of high-calorie nutrition and constant stress (stress contributes to abdominal obesity). When excess fat accumulates in the omentum, a large bulging belly appears, and the arms, legs, buttocks may remain thin.
For women, the risk of visceral obesity increases with menopause and hormonal imbalances. Of course, if you have a menopause, this does not mean that you will automatically start to get fat. The main reason, as always, is overnutrition with insufficient energy expenditure.

Despite the fact that visceral fat is deposited in the abdominal cavity for a reason, especially in women, you can get rid of it in the same ways. You will lose weight in general, and you will lose weight "there" too. These are the general laws of our body: you need to spend more energy than it enters the body.
The specific moments in getting rid of visceral fat should be considered the need to get rid of stress in your life, and learn how to go to bed on time. Excess cortisol in the body and hormonal imbalance play a role important role in this type of fat deposition.
. Your algorithm of actions is described in detail on our website.
Never go on a diet from the Internet. The fact is that in your case, the body is prone to developing insulin resistance, and if you experience metabolism swings from intermittent fasting, overloads in the form of deprivation, then an excess of carbohydrates in food, your attempts to cope with the situation will only exacerbate the problems.
In general, visceral fat is not a sentence. You can get rid of this type of obesity. Take your weight loss program seriously. Seriously - this means deliberately, we are not talking about some kind of mood for eternal starvation. You must act wisely and carefully, resorting to the help of a qualified doctor, and not prescriptions from unknown authors from the network.
Did you like the news? Share it with your friends:
Visceral fat
Visceral (internal) obesity- This is a type of obesity in which fat accumulates around the internal organs. It is located not only under the skin, but also inside the body.
Usually its weight is about 3 kg. Its task is to “warm” the organs and from time to time “nourish” with energy. But with visceral obesity, fat can reach 20 kg or more.
The dangers of visceral obesity
This type of obesity entails a number of problems.
For example, fat begins to accumulate in the area hearts. At the same time, it is compressed and stops working normally. There is a feeling of constant fatigue. The person gets tired instantly. There is increased sweating. The heart stops beating rhythmically (arrhythmia).
If fat accumulates around lungs, then breathing becomes difficult. With visceral obesity, the lungs do not fully open. Not being able to breathe deeply, the body does not receive enough oxygen to the brain cells. This prevents nerve cells from recovering. The morning feeling of cheerfulness is lost.
Likewise, fat abdominal cavity, complicates the work of the whole organism as a whole. Due to metabolic disorders, gastritis and diabetes mellitus develop.
At the same time, the risk of diabetes with visceral obesity increases by more than 50 times. Even the probability of getting cancer increases - about 15 times.
From the point of view of well-being, excess also plays a negative role. It is the "producer" of the stress hormone - cortisol. As a result, a person may experience constant psychological pressure for no apparent reason.
Another significant problem is that visceral fat "suppresses" male hormones, turning them into female ones. As a result - a decrease in sexual activity and even infertility. 
Diagnosis of obesity
There are several ways to diagnose visceral obesity.
- The easiest option is to measure the waist. If she is less 94 cm men and less 80 cm in women, everything is normal. If before 102 cm in men and 88 cm in women, it is worth paying attention. If more - you should contact a specialist;
- Another way is to calculate the ratio of the parameters of the waist and hips. For men, the normal ratio is less than 1 , for women - less 0.8 .

There are several more indices, which take into account in their "formulas" the ratio of the parameters of the arms, hips, and the like. Although, in general, the first two options are enough.
Treatment of internal obesity
Peculiarity visceral obesity is that it is almost impossible to get rid of it by conventional methods. Nor level up physical activity, neither diet nor surgery can get rid of internal obesity.
The whole point is that about half men and women with a normal body index - somehow have this problem. It is known that even some models have excess visceral fat.
Although he may be invisible, he is the most dangerous. Since it envelops the internal organs, interfering with their work.
To date no accurate medical data and recommendations on how to get rid of visceral fat. There is only statistics. According to her, people who walk slowly or otherwise for 2-3 hours a day almost never have excess visceral fat. 
So slow, but prolonged walking, jogging, moderate cycling and other non-intense long-term exercise are the best prevention of visceral obesity.
Causes in women are associated with a genetic predisposition, hormonal failure in the body, improper diet and an insufficiently active lifestyle. Let's consider each reason in detail. Let's analyze the consequences of obesity in women and how to get rid of it. extra pounds without hurting yourself.
- We recommend reading: and
The genetic predisposition of women to obesity is a common cause. Genes are responsible for appetite and metabolism in the body, for the breakdown of fats and their distribution.
But an important role here is played by the culture of food education, family lifestyle, and food preferences. If the family constantly eats, mom makes cheesecakes every day, then it is difficult for the growing generation to form a different view of the food culture.
Hormonal changes
In fact, a woman is exposed to hormonal disruptions very often: teenage changes in puberty, changes in pregnancy, menopausal syndrome. In addition, after thirty years, a woman naturally loses muscle mass and therefore, she needs less calories in consumption, and vice versa in the diet high-calorie food comes a lot. Stress also plays a significant role in obesity. A woman "jams" her problems at work or troubles in the family. Stress itself provokes hormonal failure in the body, and if you still lean on food, then obesity will definitely come!
Pregnancy and childbirth provoke a positive factor for the development of different. The fact is that during pregnancy there is a hormonal change in the body.

In order to give birth on time, and not ahead of time, there is a development a large number the female hormone progesterone. A baby in the womb requires twice the usual calorie intake. You need to eat in pregnancy for two. When a child is born, the mother's body experiences tremendous stress, which also leads to a failure at the hormonal level. In the postpartum period, lactation occurs, this factor does not allow you to choose a diet for a woman. It takes a long time to restore weight, and some will even have to resort to treatment of the disease.
Both contraceptives and antidepressants, diseases of the pituitary gland, neoplasms of the pancreas, diseases lead to a hormonal shift. thyroid gland and tumors of the ovaries, adrenal glands.
Menopause also leads to obesity of varying degrees. At this time, the endocrine system suffers, moreover, in old age, a woman has many concomitant diseases. When the body wears out, it undergoes a huge load on the cardiovascular system, muscle, metabolism suffers, which leads to disruption of the digestive tract. In addition, the elderly move very little.
Types of obesity and their consequences
What does obesity lead to? Different lead to different health problems.
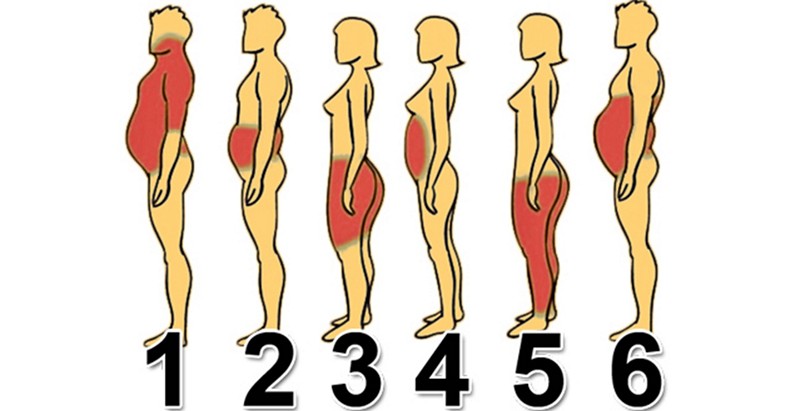
Abdominal
Most often, women suffer from abdominal, i.e. abdominal obesity. Fats are deposited in the abdomen and peritoneum. This type is not difficult to determine. In the photo, in people with abdominal obesity, the figure looks like. Here only the shape of the abdomen suffers, the rest of the body is normal at this stage.
The abdominal type of fat deposition is dangerous, because it leads to diabetes mellitus, pregnancy for a woman is impossible, hence infertility.
Abdominal obesity in women can develop into- when fatty deposits appear on the internal organs and around them. Fat begins to be localized between the fibers of the heart muscle.
Visceral obesity viewed as a threat. From the photo of such a person, we will not be able to tell about this stage of obesity, it can be determined by passing and passing the diagnosis. Inside the body, changes in the cardiovascular system occur, blood sugar rises, and the heart suffers. People who are sick with this type of obesity cannot fully move, and walking long distances gives them inconvenience, causes shortness of breath and tachycardia. If obesity gets to the uterus of a woman, then you can forget about sex life. All these reasons lead to problems of conception, pregnancy cannot occur, there will be infertility, and treatment is long.
Leg obesity
Obesity of the legs (gynoid type) This obesity (lipodystrophy) belongs to the endocrine. With such a disease, fat accumulates only on the abdomen, on the hips and in the structure of the legs.
The figure of such people resembles a pear. It causes complications from both the cardiovascular system and the skeletal system - osteoporosis, osteoarthritis.
A sufferer of this type complains of leg diseases, the inability to move. Sometimes the fat grows to such an extent that the person cannot lift their legs without assistance. The reproductive function also suffers - pregnancy cannot occur.
By male type
There is also android obesity- this is when fats are deposited in a male pattern. In the photo, this degree can be determined by the defeat of such parts of the body as the upper abdomen, chest. The shape of the legs and hips remains normal, but there is no waist.
mixed
Mixed type, when fats are distributed throughout the body of a woman. The characteristic signs of a change in this type of disease can be determined visually. The figure in the photo of such a person will be covered with body fat everywhere evenly. The shape of the abdomen, the shape of the legs, arms, back, etc. suffer.
Obesity of any type causes irreversible consequences, such as diabetes, infertility, colon and small intestine cancer.
Obesity causes menstrual irregularities - amenorrhea, which leads to the fact that a woman cannot become pregnant. Infertility in obese women is 33%, as infertility in women with normal weight is 18%.
Stages of treatment
With obesity, a woman is prescribed diagnostics and treatment. To determine the degree of obesity, calculate (BMI), body obesity index (BIO), types of obesity.
Analyzes
Be sure to conduct a laboratory study, take tests. The doctor will order blood tests for sugar and cholesterol levels.
Be sure to prescribe tests for thyroid hormones - triiodothyronine and thyrotropin. It is also important to examine the blood for prolactin, perhaps a woman's infertility lies in the deviation of this hormone from the norm.
Abdominal obesity can be manifested by low male hormone called testosterone, so testing for its presence and blood levels will be useful. Depending on what the test results will be, the degree of the disease, the doctor prescribes treatment.
Diet, exercise
For all types of obesity prescribe special diets, sports exercises aimed at the whole body as a whole and at problem areas, for example, the abdomen. Be sure to prescribe medication.
With hormonal obesity if there are testosterone deviations from the norm, a diet is prescribed where the restriction will enter. If these are the degrees of obesity in which endocrine system disorders occur, then the diet will be prescribed with sugar restriction.
Daily routine, active sports, swimming pool and daily walks will become an obligatory part of the life of an obese patient.
With obesity due to a genetic factor they also select a diet, be sure the Doctor will tell you about the right nutrition culture, prescribe sports, prescribe drugs to the woman that reduce the feeling of hunger. Although it is very difficult to fight genetic obesity, because the factor of improper vital activity, vaccinated from childhood, joins.

In order not to bring the disease to a more severe degree, a woman can also take her diet in a positive direction for health. Try to replace high-calorie foods with healthy vegetables and fruits. Large portions replace food with small ones. It may not be possible to lose weight to the desired weight, but it is quite possible to stop the growth of fat. Thus, many complications can be avoided.
Preparations
Drug treatment: prescribed, either lowering the hormone or increasing it. Depending on the level, restore its balance. For the treatment of female obesity, which provoked the factor of malnutrition and inactivity, therapy is used, as in genetic obesity. In addition to drug treatment, a nutritionist can refer a woman to a psychologist, as this is an integral part of therapy.
Psychologist's consultation
Basically, women start because of a bad psychological microclimate, which is facilitated by loneliness or separation from a spouse. In these cases, food for a woman serves as a substitute for joyful emotions. A diet prescribed by a doctor can serve as even more stress for a woman, so the problem of obesity must also be solved on a psychological level.
In cases where neither medications, nor sports, nor diets help, with obesity of degrees 3 and 4, they use a surgical method of treatment.
Liposuction
Liposuction is when fat accumulated under the skin is removed. Gastric banding, when a bandage is inserted into the stomach, thereby changing its shape. After surgery, a woman will definitely need a period of rehabilitation, which will be aimed at maintaining the psychological and emotional background of the woman, as well as at establishing the right food culture and lifestyle.
Prevention
All women, without exception, should remember that the most good method treatment of obesity will be its prevention. Obesity prevention is:
- Healthy eating (eating food that is enriched with minerals and vitamins);
- Refusal of fast foods, fatty, fried and spicy food, soda;
- Engaging in any sport (running, swimming pool, gym or fitness center);
- Daily walks in the fresh air.
OBESITY AND METABOLISM 1 "2004
literature review
Visceral obesity is a key link in the metabolic syndrome
S.A. Butrova, F.Kh. Dzgoeva
State Institution Endocrinological Research Center (Dir. - Academician of RAS and RAMS I.I. Dedov) RAMS, Moscow
The problem of obesity in combination with various metabolic disorders and/or diseases is in the focus of modern medical science and public health. The prevalence of obesity in the world is so great that it has become a global epidemic. With the spread of obesity across the planet, the associated severe somatic diseases multiply and worsen: type 2 diabetes mellitus (DM2), arterial hypertension (AH), coronary heart disease, oncological diseases, etc., which reduce the quality of life and increase the mortality rate among the working population. According to WHO experts, 320,000 people die every year from obesity-related diseases in Europe alone. The most significant medical consequences of obesity are type 2 diabetes and cardiovascular disease (CVD), and the risk of their development is largely determined by the characteristics of the deposition of adipose tissue in the body.
For the first time, J. Vague drew attention to the problem of the relationship between the risk of obesity-related diseases and the nature of the localization of adipose tissue in his writings back in 1947. He identified two types of obesity based on the topography of adipose tissue - android and gynoid - and showed that patients with android type of obesity are more likely to develop DM2, AH and CVD. Subsequent studies based on generally accepted criteria for assessing the type of distribution of adipose tissue and indicators of the risk of developing concomitant diseases proved that abdominal obesity is an independent risk factor for dyslipidemia, disorders of carbohydrate metabolism and blood coagulation, independent of the degree of obesity in general. Thus, the data of the Gothenburg study confirmed that the ratio of the circumference of the waist and hips (OT / OB) is an independent risk factor for myocardial infarction, stroke, as well as mortality from them; OT/OB has a closer relationship with these
diseases than body mass index (BMI).
With the introduction of computed tomography (CT) and magnetic resonance imaging (MRI) into medical practice, the abdominal type of obesity was divided into two subtypes - abdominal-visceral and abdominal-subcutaneous. It turned out that it is abdominal-visceral obesity that, as a rule, is combined with an unfavorable metabolic profile. In the works of J.-P. Despres, B. Wajchenberg and many other researchers have shown that the area of visceral fat in men is more than 130 cm2, and in women of pre- and postmenopausal age more than 110 cm2 indicates an increased risk of coronary heart disease. A clear correlation was found between the area of visceral adipose tissue, determined by CT and MRI, and the WC index.
A dangerous threshold for the accumulation of visceral adipose tissue - 130 cm2 in both sexes up to 40 years old - corresponds to a waist circumference of more than 100 cm, and at the age of 40-60 years - already from 90 cm. Studies by T. Han et al. , as well as other studies based on a comparison of the total health risk with indicators of waist circumference in abdominal-visceral obesity, confirmed by computed tomography, revealed that with a OT of 94-101 cm in men and 8087 cm in women, there is increased risk, and at even higher values of WC - a high risk of developing CVD and DM2. Y Matsuzava et al., using CT to determine the topography of adipose tissue in the abdominal region, showed that the accumulation of fat in visceral depots, even with normal BMI values, is usually accompanied by metabolic and hemodynamic disorders, and in 40% of patients with coronary disease heart there is visceral obesity with normal body weight.
In recent decades, various hormonal-metabolic disorders and/or diseases associated with obesity have been considered in
complex, since almost each of them, being a risk factor for the development of CVD, in combination greatly increases the risk of developing macrovascular atherosclerotic diseases. In 1988, G. Reaven described the so-called “X syndrome”, combining arterial hypertension, dyslipidemia, and carbohydrate metabolism disorders, and for the first time suggested that insulin resistance (IR) and compensatory hyperinsulinemia (GI) could be the unifying basis of these disorders. In 1989, N. Kaplan described the "deadly quartet", including abdominal obesity among the most important components of the syndrome, along with hypertension, impaired glucose tolerance, and hypertriglyceridemia. In the 1990s, metabolic disorders and diseases that develop in obese individuals were united under the "metabolic syndrome".
The meaning of introducing this concept into scientific terminology is that it combines a complex of hormonal and metabolic disorders and diseases that significantly accelerate the development and progression of atherosclerotic vascular diseases, which, according to WHO experts, occupy the first place among the causes of death in the industrialized countries of the world. Many modern researchers consider the metabolic syndrome as a prelude to diabetes mellitus.
With the development of the concept of metabolic syndrome, its scope has expanded, combining the following symptoms and manifestations:
Abdominal-visceral obesity,
insulin resistance and hyperinsulinemia,
dyslipidemia,
arterial hypertension,
Impaired glucose tolerance/type 2 diabetes mellitus,
Early atherosclerosis/CHD,
hemostasis disorders,
Hyperuricemia and gout
microalbuminuria,
Hyperandrogenism.
In recent years, many researchers have proposed to include liver steatosis and obstructive sleep apnea syndrome as components of the syndrome. The prevalence of metabolic syndrome in the general population is quite high. According to the Health and Nutrition Study (NHANESIII), conducted in the United States from 1988 to 1994 and covering almost 9000 men and women, metabolic syndrome - according to the criteria of Adult Treatment Panel III (ATPIII), was detected in 6.7% of patients in age 2029, 43.5% in the age group of 60-69 years and 42% - from 70 years and older. The specificity of the US population made it possible to identify in this study ethnic differences in the prevalence of metabolic syndrome: it occurs more often in patients of Hispanic origin (32%) compared with other ethnic groups (20-24%).
In terms of the population, the results of NHANES III showed that 24% of the population in the United States, which was about 47 million people, suffer from metabolic syndrome.
The identified ethnic characteristics of predisposition to the development of the metabolic syndrome confirm the role of genetic factors. At the same time, the growing number of patients with this pathology in all regions of the planet can be regarded as the result of the interaction of the modern lifestyle and genotypic features.
According to P. Zimmet, published in 2003, about a quarter of the population of Western European countries have impaired glucose tolerance or metabolic syndrome. The latter is most commonly found in northern European countries. According to epidemiological studies conducted in Finland and Sweden, 10% of women and 15% of men have metabolic syndrome without carbohydrate metabolism disorders.
In Russia, according to the results of the WHO MONICA study, 40% of the unorganized population of Novosibirsk aged 25-64 years have 2 or more components of the metabolic syndrome with a predominance of its prevalence among women (the definitions of this pathology developed by WHO were used in the study).
When studying the frequency of occurrence of the metabolic syndrome among obese patients who applied to the ERC of the Russian Academy of Medical Sciences, it was detected (according to the diagnostic criteria for ATP) in 49%, and in the age group from 16 to 22 years in 35% of patients.
For the first time, diagnostic criteria for the metabolic syndrome were developed and formulated by a WHO working group. However, the criteria for diagnosing ATPIII metabolic syndrome, published in 2001 by The National Cholesterol Education Program review committee, are more consistent with clinical practice (see table).
In the proposed definitions of the metabolic syndrome, an independent place is given to visceral obesity. This is justified by the results of a number of large studies that have demonstrated a close relationship between abdominal-visceral obesity and a complex of hormonal and metabolic risk factors that form the basis of the consideration.
Diagnostic criteria for metabolic syndrome
Risk factors Meaning
Abdominal obesity Waist circumference
Men > 102 cm
Women > 88 cm
Triglycerides > 3.95 mmol/l
Men< 1,1 ммоль/л
Women< 1,3 ммоль/л
BP > 130/ > 85 mm Hg Art.
Fasting glycemia > 6.1 mmol/l
OBESITY AND METABOLISM 1 "2004
a decrease in insulin binding and degradation by hepatocytes and the development of IR in the liver, inhibition of the suppressive effect of insulin on glucogenesis, as well as systemic hyperinsulinemia, which in turn contributes to the development of peripheral insulin resistance [8,9,30].
An independent effect of FFA on glycogenolysis and gluconeogenesis is also assumed.
Once in the systemic circulation, FFA contribute to impaired glucose uptake and utilization in muscle tissue through the Randle cycle and, thus, to increased peripheral insulin resistance. Excessive content of FFA in the blood serves as a source of accumulation of triglycerides and products of non-oxidative metabolism of FFA in skeletal muscles, heart muscles and, accordingly, a violation of insulin-dependent glucose utilization in these tissues. It has also been shown that FFAs have a direct toxic effect on pancreatic β-cells (the effect of lipotoxicity).
Under conditions of insulin resistance and excess FFA, lipid metabolism is disturbed and atherogenic dyslipidemia develops. Due to a slowdown in the catabolism of triglycerides and triglyceride-rich lipoproteins, increased accumulation of very low density lipoproteins (VLDL), cholesterol esters accumulate in macrophages, an increase in the level of modified low-density lipoproteins (LDL), which have a high ability to oxidize and penetrate into the subendothelial space of the vascular walls, high affinity for proteoglycans and reduced affinity for LDL receptors. All these properties contribute to the active inclusion of small dense particles of LDL in the process of atherogenesis.
Along with impaired lipid metabolism under conditions of insulin resistance and hyperinsulinemia, there is an increase in the proliferation of smooth muscle cells, fibroblasts, and collagen synthesis, which also contribute to the development of atherosclerotic vascular lesions.
Among the adipokines secreted by adipose tissue and affecting the development of the components of the metabolic syndrome, leptin, tumor necrosis factor-a, and adiponectin are currently the most studied.
Leptin is a multifunctional adipose tissue hormone secreted by adipocytes in proportion to the mass of adipose tissue. The effect of leptin on the central nervous system, a number of neuroendocrine functions, immune system, bone metabolism, lipid and carbohydrate metabolism (Fig. 1). The leading function of leptin, as shown by recent studies, is the protection of peripheral tissues from ectopic lipid accumulation. According to H. Unger and L. Orci, leptin is an antisteatogenic hormone and, like insulin, which regulates glucose homeostasis and prevents the development of glucotoxicity, regulates homeostasis fatty acids, protecting against the development of lipotoxicosis. The effect of leptin on insulin resistance has been
Absorption and metabolism of glucose
, . ----------------------------------► Leptin
- absorption of glucose
Fat deposition and fat metabolism / Homeostasis
glucose tissue
Rice. 1. Effects of leptin.
torn syndrome. The close relationship between abdominal obesity and cardiovascular risk factors has allowed ATP specialists to define the metabolic syndrome as a set of metabolic complications of obesity. Primary insulin resistance and compensatory hyperinsulinemia are the key link that unites various disorders that develop in the metabolic syndrome.
The pathogenesis of IR in visceral obesity is heterogeneous and is determined by the interaction of a number of factors: genetic, gender, age, hormonal influences, conditions of intrauterine development, external influences, etc. Research results recent years showed that adipose tissue secretes a number of active molecules - adipokines that affect food intake, metabolic processes, the formation of oxidative stress and disorders of the cardiovascular system, i.e., having various local, peripheral and central effects. Many studies emphasize that in obesity, the development and progression of insulin resistance and its various manifestations may be a reflection of the lipotoxic effects of free fatty acids and an imbalance of adipokines. Therefore, adipose tissue itself, providing a large amount of FFA and cytokines to the bloodstream, is a key factor in the development of major disorders and manifestations of the metabolic syndrome.
According to many researchers, the topographic and metabolic features of visceral adipose tissue are decisive in the development of insulin resistance and complications of obesity (portal theory).
With the predominant deposition of fat in the visceral region, FFAs released due to intensive lipolysis in large quantities enter the portal vein and liver. It leads to
revealed by studying metabolic parameters in leptin deficiency syndromes, which are accompanied by hyperphagia, obesity, hypercortisolemia and type 2 diabetes. The introduction of exogenous leptin contributed to the normalization of metabolic parameters, regardless of the dynamics of body weight, which served as the basis for the conclusion about the independent role of leptin in the impact on insulinemia and insulin resistance.
A number of authors do not exclude the possible effect of leptin on insulin sensitivity through a direct effect at the level of peripheral tissues. In visceral obesity, the combination of elevated plasma concentrations of FFA, triglycerides, LDL, chylomicrons and peripheral leptin resistance, which develops against the background of hypercortisolemia, leads to the deposition of fatty acids in the form of triglycerides in skeletal muscles, liver, heart muscle, and pancreas. Excessive deposition of triglycerides in organs is a potential source of FFAs entering the cells in an amount that significantly exceeds their oxidative needs.
Normally, with an excess intake of fatty acids in tissues, the activity of FFA oxidation enzymes increases, and unused energy is dissipated in the form of heat with the help of acyl-CoA reductase and UCP-2, that is, the system of the so-called compensatory FFA oxidation is activated. It is obviously enhanced by the FFAs themselves, which are ligands of PPAR-y, which increases the expression of enzymes at the final stages. this process. This compensatory oxidation system requires normal functioning leptin systems. With leptin resistance, compensatory oxidation of FFA does not occur, the non-oxidative pathway of their metabolism (peroxidation and the formation of ceramides) is activated. The accumulation of unoxidized metabolites of free fatty acids and ceramides can stimulate the development of lipotoxic disorders, end result which are manifestations of the metabolic syndrome: insulin resistance, hyperlipidemia, diabetes mellitus, cardiomyopathy, increased blood pressure(HELL). When the action of leptin is impaired, there is also an increase in the synthesis of de novo fatty acids from glucose due to overexpression of a number of proteins involved in the process, and this synthesis occurs regardless of the concentration of FFA.
Under conditions of visceral obesity and leptin resistance, the effect of leptin on vascular calcification, accumulation of cholesterol by macrophages, initiation of oxidative stress, and increased tone of the sympathetic nervous system, increased blood pressure. All these factors together reduce the compliance of arteries with respect to atherosclerotic processes. Thus, in visceral obesity, leptin disruption may be one of the leading factors in the development of insulin resistance, dysfunction of β-cells, and atherogenesis processes.
Adiponectin-
Oxidation
FFA oxidation| 3 Glucose| TG|
Vascular h ¡
i inflammation
Insulin sensitivity t
Rice. 2. Proposed effects of adiponectin.
One of unique products secreted by adipose tissue is adiponectin. However, unlike other adipokines, the secretion of which increases in proportion to the increase in adipose tissue mass, its level in obese people is lower than in people with normal body weight. The obtained experimental data demonstrated the inhibitory effect of adiponectin on the differentiation of pre-adipocytes, which confirms its possible impact on the regulation of body fat. TNF-a, interleukin-6 (IL-6), and PPARY are involved in the expression and secretion of adiponectin itself. Multicenter studies have shown that plasma adiponectin levels are inversely related to obesity, adipose tissue mass, WC/VR, dyslipidemia, cardiovascular disease, and insulin resistance.
A decrease in adiponectinemia has a stronger correlation with hyperinsulinemia and insulin resistance than with overall obesity and adipose tissue mass. A prospective study among Pima Indians found that low plasma levels of adiponectin preceded the onset of insulin resistance. The experiment showed that adiponectin helps to reduce insulin resistance by stimulating tyrosine phosphorylation of the insulin receptor, and also reduces the supply of fatty acids to the liver and stimulates their oxidation by activating protein kinase, helping to reduce glucose production by the liver and the synthesis of VLDL triglycerides. In muscle tissue, adiponectin, like leptin, stimulates FFA oxidation, reduces intramyocellular lipid accumulation, and improves insulin sensitivity of muscle tissue (Fig. 2). It is possible that adiponectin stimulates FFA oxidation by expressing the genes encoding CD36, acyl-CoA oxidase, and iCP-2, as well as by activating AMP protein kinase.
OBESITY AND METABOLISM 1 "2004
OBESITY AND METABOLISM 1 "2004
As part of a prospective study of cancer and nutrition in Europe (European Prospective Investigation into Cancer and Nutrition), it was found that low levels of adiponectin have an independent correlation with an increased risk of developing T2DM in relatively healthy people. The results of scientific work have given grounds for many researchers to consider adiponectin as a marker of insulin resistance in patients with type 2 diabetes.
Clinical studies have also shown that low levels of adiponectin are associated with an atherogenic lipid profile and high blood pressure. M. Matsubara et al. found that in women without carbohydrate metabolism disorders, the concentration of adiponectin in blood plasma has a clear negative correlation with the atherogenic index (TC/HDL cholesterol), triglyceride levels and apolipoproteins B and E, as well as a positive correlation with HDL and apoprotein A-1.
K. Hotta et al. reported a pronounced negative correlation of adiponectin levels with triglycerides and a positive correlation with HDL in patients with type 2 diabetes. It was also shown that in patients with type 2 diabetes and CAD, the level of adiponectin is lower than in patients without CAD, which may indicate its antiatherogenic properties. Hypoadiponectinemia, which is present in patients with metabolic syndrome, may contribute to the growth of atherosclerotic changes in them. The administration of recombinant adiponectin to such patients leads to an increase in the inhibitory effect of insulin on gluconeogenesis. This effect is associated with a decrease in the expression of such gluconeogenesis enzymes as glucose-6-phosphatase and phosphoenolpyruvate carboxykinase.
The relationship found between low levels of adiponectin, obesity, insulin resistance, coronary artery disease, and dyslipidemia allows us to consider adiponectin as another marker of the metabolic syndrome.
The works of Japanese scientists have shown that adiponectin inhibits platelet adhesion to the endothelium, inhibits the transformation of macrophages into foam cells, inhibits the proliferation and migration of myocytes, the capture of LDL by the forming atherosclerotic plaque, inhibits the activity of myelomonocytes, phagocytes, and reduces the production of TNF-a by macrophages. Moreover, adiponectin has been found to have an inhibitory effect on growth factor-mediated proliferation of smooth muscle cells in the aorta.
Physiological concentrations of adiponectin suppress the expression of adhesive molecules. One of the most important anti-atherogenic mechanisms of action of adiponectin - inhibition of monocyte adhesion to the endothelium - occurs due to a decrease in the activity of the nuclear transcription factor kappa B (NTP-kB), blocking the phosphorylation of its I-kB subunit. Moreover, adiponectin has been found to have an inhibitory effect on growth factor-mediated proliferation of smooth muscle cells in the aorta. The listed protective
The specific mechanisms of adiponectin in relation to the development of atherosclerosis are lost in obesity, especially in its abdominal-visceral subtype. In addition, visceral adipose tissue secretes a number of cytokines that inhibit the action of adiponectin, the main of which is tumor necrosis factor-a.
Many publications have noted a positive correlation between the expression of TNF-a and the values of WC/RT, BMI, systolic blood pressure, as well as a decrease in the expression of TNF-a and its concentration in the blood with a decrease in body weight. The mechanism of action of TNF-a on insulin sensitivity is to reduce the activity of the insulin receptor tyrosine kinase and increase the phosphorylation of serine, the substrate of the insulin receptor, as well as to inhibit the expression of GLUT-4 in muscle and adipose tissue. TNF-a also inhibits adipocyte differentiation. It is believed that this cytokine has an auto- and paracrine effect and is of the greatest importance for the development of insulin resistance in adipose tissue. TNF-a may also contribute to the development of insulin resistance by stimulating lipolysis in adipocytes.
In obesity, TNF-a plays an important role in increasing the expression of plasminogen activator inhibitor-1 (PAI-1), the production of leptin, interleukin-6, and reducing the expression and activity of adiponectin. TNF-a stimulates the activation of the nuclear transcription factor kappa B, which increases the production of NO - the basis of the inflammatory response in the vascular wall, intracellular adhesion of monocytes and the entire oxidative stress cascade. One of the effects of JTP-kV is the impairment of the insulin receptor signal and the development of insulin resistance.
It has been shown that in proportion to the increase in the mass of adipose tissue in the blood, the concentration of interleukin-6 increases. The production of interleukin-6 by the adipose tissue of the omentum is 2-3 times higher than that of the subcutaneous abdominal adipose tissue. Due to the specific location of visceral adipose tissue, IL-6 secreted by it has the ability to directly affect metabolic processes in the liver by suppressing the sensitivity of liver insulin receptors. This adipokine stimulates the formation of C-reactive protein, which is a marker of the inflammatory process of the vascular wall. IL-6 reduces the expression of lipoprotein lipase, exerting a local effect on the absorption of FFA by adipocytes, increases the production of triglycerides, which may be important for the development of hypertriglyceridemia in visceral obesity. This cytokine also has a direct stimulatory effect on the hypothalamic-pituitary-adrenal system and has a positive correlation relationship with insulin resistance, the development of type 2 diabetes, and myocardial infarction. It has been established that in patients with abdominal obesity, the adipose tissue of the omentum is the main source of elevated plasma levels of in-
plasminogen activator-1 inhibitor. At normal body weight, PAI-1 synthesis occurs mainly in hepatocytes and endothelial cells, and to a lesser extent in smooth muscle cells and platelets. PAI-1 is a serine protease inhibitor and the main regulator of the fibrinolytic system. It binds and inhibits tissue-type plasminogen activators and urokinase, which modulate endogenous fibrinolysis. As many authors testify, a high level of PAI-1 is an independent predictor of myocardial infarction in men with coronary artery disease. A number of prospective studies have shown a relationship between increased level PAI-1 and the risk of developing atherosclerosis and thrombosis, especially coronary. In obesity, there is an increased expression of the PAI-1 gene and a clear positive correlation between the level of PAI-1 and the parameters of the metabolic syndrome, especially between the level of fasting glucose and insulin, triglycerides, LDL cholesterol, visceral adipose tissue mass and BMI.
In 2001, a polypeptide was isolated - resistin, which is secreted mainly by preadipocytes and, to a lesser extent, by mature adipocytes, mainly of abdominal localization. Experiments have shown that the administration of recombinant resistin to non-obese mice leads to the development of insulin resistance, and the administration of antiserum to resistin improves insulin sensitivity in animals with obesity and IR. According to experimental data, resistin neutralizes the inhibitory effect of insulin on glucose production by the liver and reduces glucose uptake by skeletal muscles, regardless of GLUT-4. However, the role of resistin in the mechanisms of IR development is still not clear enough: there are works in which it was not possible to confirm its role in the pathogenesis of insulin resistance in obesity. In addition, most of the known mechanisms of action of resistin were found in experiments with mice, and human resistin is similar in structure to mouse resistin only by 59%.
It has been established that adipose tissue is the second source of angiotensin secretion after the liver, and its expression is more pronounced in visceral than in subcutaneous adipocytes. Enzymes that convert angiotensinogen to angiotensin I and angiotensin II are also expressed in adipose tissue. Angiotensin II, produced by adipose tissue, accelerates the differentiation of preadipocytes into adipocytes by stimulating the production of prostaglandin K. It is also suggested that increased production of angiotensinogen through angiotensin II may play a role in the mechanisms of arterial hypertension in obese patients. Angiotensin II is a proatherogenic protein that stimulates intracellular adhesion of molecules to the vascular wall, the formation of free radicals, and disruption of the integrity of the vascular wall. All these processes provoke endothelial dysfunction.
Almost all components of the metabolic syndrome are abdominal-visceral obesity,
Mechanisms of development of type 2 diabetes mellitus and atherosclerosis in obesity
(after Ch. Lyon, R. Law and Whsueh, 2003)
insulin resistance
metabolic syndrome
Diabetes type 2
Endothelial dysfunction
f Oxidative stress f Inflammatory response f Atherosclerosis
f f f Atherosclerosis
IR and GI, dyslipidemia, AH, IGT/DM-2, early atherosclerosis/CHD, hemostasis disorders, hyperuricemia and gout, microalbuminuria, hyperandrogenism
They are established risk factors for the development of cardiovascular diseases, their combination greatly accelerates the development of CVD.
Recently, in connection with the in-depth study of the molecular mechanisms of the inflammatory reaction of the vascular wall in the pathogenesis of atherosclerotic plaque formation, the influence of the nuclear transcription factor kappa B has attracted increasing interest. angiotensinogen II directly or indirectly stimulate the activation of JTP-kV, which provokes endothelial dysfunction, an inflammatory cascade of cytokines, the formation of oxidative stress on the vascular wall, leading to the formation of atherosclerotic changes and the development of insulin resistance. The only protective factor, adiponectin, in addition to reducing its amount and activity in visceral obesity, is suppressed by the action of a number of cytokines (see diagram).
Thus, the disorders that accompany visceral obesity are interconnected with each other like links in a "vicious circle" when an unfavorable change in one can lead to an aggravation of the other, and ultimately to the development of the metabolic syndrome.
OBESITY AND METABOLISM 1 "2004
OBESITY AND METABOLISM 1 "2004
Literature
1. Butrova S. A. Metabolic syndrome: pathogenesis, clinic, diagnosis, approaches to treatment. RMJ 2001; 2(9):56-60.
2. Dedov I. I., Suntsov Yu. I., Kudryakova S. V. Epidemiology of diabetes mellitus. In: Diabetes mellitus. Guide for doctors. - M. - Universum pub-leashing 2003; 75-93.
3. Melnichenko G.A. Obesity in the practice of an endocrinologist. breast cancer. 2001; 2(9): 82-87.
4. Nikitin Yu. P., Kazeka G. R., Simonova G. I. The prevalence of metabolic syndrome X components in an unorganized urban population (an epidemiological study). Cardiology 2001; 9:37-40.
5. Auwerx J, Mangelsdorf D. X-ceptors, nuclear receptors for metabolism. Excerpta Medica, Atherosclerosis XII 2000: 21-40.
6. Beck-Nielsen H. General characteristics of the insulin resistance syndrome: prevalence and heritability European Group for the study of Insulin Resistance (EGIR). Drugs 1999; 58:5-7.
7. Bergman R. Non-esterified fatty acids and the liver: why is insulin secreted into the portal vein? Diabetology 2000; 43:946-953.
8. Boden G, Shulman G.I. Free acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and in-cell dysfunction. Eur J Clin Invest 2002, 32 (Suppl 3): 14-23.
9. Bollheimer L, Skelly R, Chester M, McGarry J, Rhodes C. Chronic exposure to free fatty acid reduces pancreatic beta cell insulin content by increasing basal insulin secretion that is not compensated for by a corresponding increase in proinsulin.
10. Chandron M., Phillips S. A., Ciaraidi T., Henry R. R. Adiponectin: more than just another fat cell hormone? Diabetes Care 2003; 26:2442-50.
11. Despres J-P, Marette A. Relationship of components of insulin resistance syndrome to coronary disease risk. Curr Opin Lipidol 1994; 5:274-289.
12. Despres J-P. Inflammation and cardiovascular disease: is abdominal obesity the missing link? Int J Obes 2003, 27 (Suppl): 22-24.
13. Gillum R, Mussolino M, Madans J. Body fat distribution, obesity, overweight and stroke incidence in women and men: the NHANES I Epidemic Follow-up Study. Int J Obes Relat Metab Disord 2001; 25:628-638.
14. Goossens GH, Blaak EE, van Baak MA. Possible involvement of the adipose tissue renin-angiotensin system in the pathophysiology of obesity and obesity-related disorders. Obesity Rev 2003, 4:43-55.
15. Han T, van Leer E, Seidell J, Lean M. Waist Circumference Abdominal Sagittal Diameter. Best Simple Anthropometric Indexes of Abdominal Visceral Adipose Tissue Accumulation and Related Cardiovascular Risk in Men and Women. Am J Cardiol 1994; 73; 460-468.
16 Hauner H, Petruschke T, Russ M, et al. Effects of tumor necrosis factor alpha (TNFa) on glucose transport and lipid metabolism of newly differentiated human fat cells culture. Diabetologia 1995, 38: 764-771.
17. Hern_ndez-Rodriguez J, Seragga M, Vilardell C, et al. Elevated production of interleukin-6 is associated with a lower incidence of disease-related ischemic events in patients with giant-cell arteritis. Angiogenic activity of interleukin-6 as a potential protective mechanism. Circulation 2003, 107: 2428-2434.
18. Joseph NA, Greenberg AS. Adipocytokines and insulin resistance. J Clin Endocrinol Metab 2004, 89(2): 447-460.
19. Juhan-Vague I, Alessi C, Vague P. Thrombogenic and Fibrinolytic Factors and Cardiovascular Risk in non-insulin-dependent Diabetes Mellitus. The Finnish Medical Society DUODECIM, Ann Med 1996; 28:371-380.
20. Juhan-Vague I, Stephen D, Pyke M et al. Fibrinolytic Factors and the Risk of Myocardial Infarction or Sudden Death in Patients With Angina Pectoris. Circulation 1996; 94:2057-2063.
21. Kalkhoff RD, Hartz AJ, Ruplay DC, Kissebah A, Kelber S. Relationship of body fat distribution to blood pressure, carbohydrate tolerance, and plasma lipids in healthy obese women. J Lab Clinic Med 1983; 102:621-627.
22. Kissebah A, Krakower G. Regional adiposity and morbidity. Physiol Rev 1994; 74:761-811.
23. Lapidus L, Bengtsson C, Larsson B, Pennert K, Rybo E, Sj_str_m L. Distribution of adipose tissue and risk of cardiovascular disease and death: a 12-year follow-up of participants in the population study of women in Gothenburg, Sweden. BMJ 1984; 289:1261-1263.
24. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation 2002,
25. Lindsay RS, Funahashi T, Habson RL et al. Adiponectin and development of type 2 diabetes in the Pima Indian population. Lancet 2002, 360: 57-58.
26. Maeda N, Takanashi M, Funahashi T et al. PPARy ligands increase expression and plasma concentration of adiponectin, an adipose-derived protein. diabetes
2001, 50: 2094-2099.
27. Matsubara M, Maruoka S., Katayose S. Decreased plasma adiponectin concentrations in women with dyslipidemia. J Clin Endocrinol Metab 2002; 87:2764-9.
28. Matsuzawa Y., Funahashi T., Nacamura T. Molecular mechanism of metabolic syndrome X: contribution of adipocyte-derived bioactive substances. Ann N Y Acad Sci 1999; 892:146-54.
29. Mohamed-Ali V, Pinkney JH, Coppack SW. Adipose tissue as an endocrine and paracrine organ. Int J Obes Relat Metab Disord 1998, 22: 1145-1158.
30 Neel J, Julius S, Weder A et al. Syndrome X: is it for real? Genet Epidemiol 1998; 15:19-32.
31 Okamoto Y, Arita Y, Nishida M et al. An adipocyte-derived plasma protein, adiponectin, adheres to injured vascular walls. Horm Metab Res 2000, 32:47-50.
32. Ouchi N., Kihara S, Nishida M et al. Adipocyte-derived plasma protein, adiponectin, suppress lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation 2001, 103: 1057-1063.
33. Ouchi N., Kihara S., Arita Y. et al. Adiponectin, adipocyte-derived plasma protein, inhibits endothelial NF-kB signaling through camp-dependent pathway. Circulation 2000, 102: 1296-1301.
34. Ouchi N., Kihara S., Arita Y. et al. Novel modulator for endothelial adhesion molecules: adipocyte-derived plasma protein adiponectin. Circulation 1999; 100:2473-6.
35. Pajvani UB, Scherer PE. Adiponectin: systemic contributor to insulin sensitivity. Curr Diab Rep 2003, 3:207-213.
36. Porter MH, Cuthins A, Fine JB, et al. Effects of TNF-a on glucose metabolism and lipolysis in adipose tissue and isolated fat-cell preparations. J Clin Med 2002, 139: 140-146.
37. Rabinovitch A, Suares-Pinzon WL. Cytokines and their roles in pancreatic islet ß-cell destruction and insulin-dependent diabetes mellitus. Biochem Pharmacol 1998, 55: 1139-1149.
38. Reaven G. M. Banting Lecture: the role of insulin resistance in human disease. Diabetes 1988; 37: 1595-1607.
39. Rexrode K, Buring J, Manson J. Abdominal and adiposity and risk of coronary heart disease in men. Int J Obes Relat Metab Disord 2001; 25:1047-1056.
40 Sonnenberg GE, Krakower GR, Kissebah AH. A novel pathway to the manifestations of metabolic syndrome. Obesity Research 2004, 12(2): 180-192.
41 Spranger J, Kroke A, M_hlig M et al. Adiponectin and protection against type 2 diabetes mellitus. Lancet 2003, 361: 226-228.
42. Sun Z, Andersson R. NF-kB activation and inhibition: a review. Shock 2002, 18:99-106.
43 Takanashi M, Funahashi T, Shimomura I et al. Plasma leptin levels and boby fat disribution. Horm Metab Res 1996, 28:751-752
44. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). NIH Publication 2001; 5. No. 01-3670.
45. Unger R H. Lipotoxic Diseases. Annu Rev Med 2002; 53:319-36.
46. Vague J. La diff_renciation sexuelle, facteur d_terminant des forms de l'obesit_. Presse Med 1947; 30:339-340.
47. Vanhala M G, Pitkajarvi T K, Kumpusalo E J, Takala J K. Metabolic syndrome in middle-aged Finnish population. J Cardiovasc Risk 1997; 4:291-5.
48. Weyer C, Funahashi T, Tanaka S, et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 2001, 86: 1930-1935.
49 Yokota T, Rreddy Mekka, Medina K L et al. Paracrine regulation of fat cell formation in bone marrow cultures via adiponectine and prostaglandins. J Clin Invest
2002, 109: 1303-1310.
50. Zinman B, Hanley A J G, Harris S B et al. Circulating tumor necrosis factor-a concentrations in a native Canadian population with high rates of type 2 diabetes mellitus. J Clin Endocrinolol Metab 1999, 84: 2172-2178.