Some are interested in why a rash appears with HIV and how to distinguish allergic reactions from a symptom of the disease. The occurrence of a rash with HIV is considered a fairly common occurrence. It is also one of the first signs of the onset of the disease. Various rashes and spots on the human body are a sign of ingestion and the development of infection. Of course, it is impossible to make an unpleasant diagnosis purely on this basis, therefore it is necessary to know what the skin lesion looks like with HIV infection and how to distinguish an allergic reaction from a symptom of the disease.
The skin is a natural mirror of the state of the human body. In the event of any changes and pathologies in the systems and organs, you can immediately notice the damage to the skin and mucous membranes.
As for HIV infections, they can provoke a variety of skin diseases. Among them are the following:
- infectious;
- neoplastic;
- various types of dermatoses, the origin of which is not fully known.
All of the above skin lesions have unusual symptoms and manifestations, in addition, they are very difficult to treat.
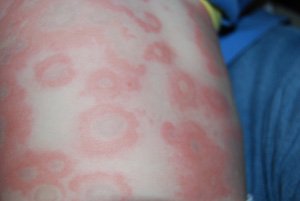
If we turn to statistics, then in about a quarter of cases when infected with HIV, the patient can observe an active manifestation of the disease at 2-8 weeks. Symptoms of the manifestation of infection will be: fever, diarrhea, inflammation of the tonsils, pain in the muscles, inflammation in the lymph nodes. Plus, a symmetrical rash will begin to appear on the skin of a person, which is easy to confuse with syphilitic roseola or rashes with measles. The main place of localization of the rash is the human torso. These can be spots on the neck, face, back and other parts. Various spots and pimples can last on the skin for 3 days or 3 weeks.
In the case when the patient has an exacerbation of the disease, so-called hemorrhagic spots can be seen on the body as rashes. They are very similar to the manifestation of allergies and have a diameter of about 3 mm. With HIV infection, as a rule, such a symptom is accompanied by a violation of the integrity of the mucous membranes of the mouth and esophagus. In addition, cases of viral skin lesions are not uncommon, for example, the manifestation of herpes or.
Exacerbation of HIV can be within a few days, or even for 2 months. After this period, all the above symptoms will disappear, skin rashes will disappear, and the disease will go into a latent phase, the duration of which cannot be predicted. Of course, during the period of attenuation of the disease, the patient is not immune from the occurrence of various fungal and viral infections that also appear on the skin. At the same time, HIV infection will complicate the treatment and the process of rehabilitation of the body after any disease.
In more rare cases, in approximately 10% of patients, seborrheic eczema or dermatitis is considered. This skin disease is typical for the period of attenuation of the disease. However, even with actively developing AIDS, such a skin lesion can be detected, while all other symptoms can remain hidden for several years. Localization of rashes of this nature is observed on the human body in places of accumulation most sebaceous glands. This face (especially cheeks), top part trunk, scalp.

Skin lesions
Herpes is one of the most common skin diseases. It also occurs in people who are HIV-infected. Most often, in such patients, the manifestation of herpes simplex is observed in the area around the mouth or on the genitals. Exacerbations are not uncommon, in which non-healing ulcers develop at the site of the rash.
In the presence of HIV infection in the human body, cases of pyoderma are not uncommon. Such a skin disease is characterized by the manifestation of follicles, which, according to appearance reminiscent of acne or teenage acne. Pyococcal diseases are also considered characteristic symptoms of HIV. Among them, vegetative, diffuse or chancriform pyoderma can be distinguished.
It's no secret that HIV infection is associated with dysfunction various systems in the human body. Therefore, in violation of the function of the vessels, rashes immediately appear on the mucous membranes and skin of the patient. It may be a hemorrhagic rash, which has a dense localization on the chest.
More than half of HIV patients know firsthand about seborrheic dermatitis. This disease manifests itself in the early stages. In this case, the clinical picture in patients may be different. The rash is characterized by both strictly limited elements on the skin, and lesions of large localization. Over time, pathological processes begin to progress, and a patient with HIV may notice uncharacteristic places for the spread of seborrheic dermatitis spots (stomach, limbs, sides).
If seborrheic dermatitis in AIDS is characterized by non-standard localization, then papular rash is characterized by small sizes and foci of appearance. The skin in the process of developing the disease will not change color or become reddish, the surface will be smoothed and dense. The papular rash in HIV is characterized by individual patches on the body that do not merge and are localized on the neck, head, limbs, and upper body. The main symptom in this case disease there will be severe itching of the affected areas.
With HIV infection, very often the patient suffers from rubrophytosis and candidiasis, multi-colored lichen and inguinal epidermophytosis.

One of the most characteristic diseases for the manifestation of HIV symptoms is considered. This is a very long dermatitis that can accompany the patient for several years. Most often, Kaposi's sarcoma affects young people. The elements of the rash are characterized by a bright color and rapid dissemination. This disease is known for the fact that it progresses very quickly, instantly affects the internal organs and lymph nodes.
Signs of dermatitis
It is one thing when dermatitis is a separate disease and amenable to traditional methods of treatment, but when an HIV infection occurs in the body, any skin disease acquires its own characteristics. For example, spots and rashes are more resistant to medicines, have a more severe course, constantly progress on the skin of the patient. In some cases, HIV dermatitis is accompanied by lymphadenopathy, has unusual locations on the human body, and other clinical manifestations.
Prevention
most important role has a constant diagnosis and the passage of various tests to detect infection. All people who are donors of blood, organs, sperm, and tissues should be examined.
It is important for every person to know the rules for preventing infectious diseases and to undergo an annual free examination using special tests or analyzes.
A rash with HIV is considered one of the symptoms of the disease that appears in the early stages. Of course, making a final diagnosis based on this symptom is impossible, but the appearance of specific rashes becomes a reason to see a doctor.
Skin lesions
Any rash on the skin caused by a viral infection is called an exanthema. Enanthems - rashes on the mucous membranes of an infectious origin. They develop under the influence of various negative factors. Enanthems are frequent companions of the early stages of HIV infection. They can also occur in a person who is HIV-negative. The rash that occurs against the background of immunodeficiency has several distinctive features that are not characteristic of dermatological diseases in people with normal immunity.
Against the background of immune suppression, skin diseases of an infectious and malignant nature, dermatoses of unknown origin often develop. Any concomitant disease of HIV infection will be manifested by an atypical clinical picture. All skin lesions in this case are characterized by a protracted course, bacteria and fungi quickly develop resistance to drugs, which complicates the treatment process. If a rash is found on the body of an HIV-infected person, it is necessary to determine its nature and origin. Often, skin rashes are similar to manifestations of measles, allergic dermatitis, herpes zoster, or syphilis.
The most acute manifestation of skin rashes occurs 2-8 weeks after infection. Acute exanthems are most often found on the skin of the trunk and face. Particular attention should be paid to other symptoms that accompany the onset of a rash. With HIV infection, swollen lymph nodes, chills, sweating, and diarrhea are often noted. These manifestations are very similar to those of influenza and viral mononucleosis. With HIV infection against the background of a progressive decrease in immunity, the patient's condition only gets worse over time. Rashes capture more and more areas, a herpetic rash appears, papules and bullae appear at the same time.
If skin lesions begin with single rashes, then over time they turn into multiple ones, gradually spreading to the whole body.
Dermatoses
Rubrophytosis is a skin disease characterized by a variety of clinical manifestations. As a rule, rubrophytosis leads to the appearance of weeping eczematous rashes, keratoderma of the palms and feet, seborrheic dermatitis and papular rash. Multicolored lichen is no less frequent companion of HIV infection. Initially, spots appear on the skin, which eventually turn into multiple rashes.
To skin rashes of viral origin include herpes. Most often, spots appear on the mucous membranes of the genitals, the skin of the lips and the perianal region. Unlike people with normal immunity, HIV-infected people suffer from more severe forms of the disease. Rashes affect large areas, periods of remission in some cases are absent. Ulceration of herpetic rash leads to the attachment of a bacterial infection and the occurrence of severe pain.

Against the background of a decrease in immunity, other changes in the condition of the skin may appear. Pyodermatitis is represented by a wide range of rash types. The most common are folliculitis, impetigo, microbial eczema. At HIV infection functions are broken of cardio-vascular system, due to which the general condition of the mucous membranes and skin changes. Most often, such changes are in the nature of erythema, spider veins and areas of hemorrhage.
Seborrheic dermatitis is found in half of those infected, it usually appears in the early stages of infection. In the later stages of HIV, dermatitis has a severe protracted course. Symptoms may vary. Dermatitis manifests itself both in a short-term localized form and in a long-term general one. Papular rashes have the appearance of small elevations on the skin, which have a dense structure and flesh color. Such a skin lesion is a single, unrelated rash in the face, arms, trunk and neck. The rash is accompanied by intense itching.
It is an undeniable symptom of human infection with HIV infection.
In this case, it has a pronounced clinical picture: an intensely colored rash occurs in areas atypical for sarcoma - on the skin of the trunk and face, the mucous membranes of the genital organs and the oral cavity. The disease proceeds in an aggressive form, quickly affecting the lymphatic and other systems of the body. All types of skin rash in HIV infection are accompanied by an increase in lymph nodes, have an atypical clinical picture, a long course and frequent relapses.
The problem of HIV infection is widespread all over the world today. This disease is incurable, therefore, a particularly important method of dealing with it is timely diagnosis and the appointment of adequate treatment. One of the main signs is the presence of specific rashes in patients.
Types of rash with HIV
Skin rashes with HIV appear at the earliest stages and are a significant symptom that allows you to suspect this disease.
These include:
Fungal lesions of the skin and mucous membranes
The hallmarks of HIV are: the rapid appearance of lesions on large areas of the body, spread to the scalp, resistance to treatment, the severity of the course, reappearance after treatment.
There are 3 forms:

- rubrophytia- a disease manifested in the formation of the following elements on the skin: exudative erythema, seborrheic dermatitis, keratoderma of the palms and soles, papular rash. It may be represented by one or more of the features described above.
- versicolor versicolor- in HIV-infected people, it occurs in the form of a rash, represented by red spots about 2-4 cm in diameter, turning into pustules and plaques.
- mucosal candidiasis. The peculiarity lies in the defeat of organs atypical for healthy people - the trachea, bronchi, urinary tract, genitals, oral cavity. Not cured by conventional antifungal agents, relapses and secondary infection often occur.
Viral lesions, predominantly mucous membranes
- herpes simplex and herpes zoster. Often manifested in the oral cavity, genitals, anal area. It is difficult to cure and has a tendency to reappear. Severe and painful course, elements of the rash almost always ulcerate.
- molluscum contagiosum- appears on the face, especially often on the skin of the forehead and cheeks, has the appearance of reddish nodules with an impression on the top.
- hairy leukoplakia- usually occurs in the oral cavity, indicates a strong weakening of the immune system.
- pointed papillomas and condylomas, common warts - are formed on the genitals and in the anal area.
Kaposi's sarcoma
Kaposi's sarcoma - is a malignant vascular tumor that can affect internal organs or skin. It has the appearance of red-violet spots, at first small in size. Later, they merge, a dense conglomerate is formed, which affects nearby tissues and lymph nodes.
The disease develops very quickly, affecting mainly young people. It is one of the pathognomonic (indicator) symptoms of HIV infection.
Purulent skin lesions or pyodermatitis
They proceed according to the type of juvenile acne, they are resistant to any ongoing treatment. Characterized by streptococcal infection.
Distinctive features of the rash with HIV
The course of a rash in the presence of HIV infection in the body has a number of distinctive features:
- Process Generalization- the spread of rashes to large areas of the body or to several areas (for example, on the head, neck and back).
- Rapid appearance of rash elements(may develop in several areas within 5-7 days).
- Severe clinical course(soreness, there may be a high temperature), frequent ulceration of the primary elements of the rash, the addition of a secondary infection (formation of pustules).
Poorly amenable to standard therapy (antifungal, antiviral), the appointment of potent drugs from the same group is required. Relapses almost always occur after treatment.
Stages of HIV infection
HIV infection occurs in several stages:
Incubation period
From the moment the virus enters the bloodstream until the first clinical signs appear in the body. It can last on average from 2 weeks to 1 month. At this time, the virus multiplies in the human body.
The appearance of the first clinical signs
Follows the incubation period. The virus accumulates in sufficient quantities, which is accompanied by the release of antibodies to it and the body's reaction to it.
It is divided into 3 stages:
- 2A - acute febrile stage- in its manifestation it is similar to a catarrhal disease: weakness, malaise occurs, body temperature rises, there is an increase in lymph nodes in many parts of the body. After 1-2 weeks, these signs disappear.
- 2B - asymptomatic stage- characterized by the complete absence of any clinical symptoms. Most often it lasts for several years.
- 2B - stage of persistent generalized lymphadenopathy- there is a gradual reproduction and accumulation of the virus in the body and cell damage immune system(lymphocytes). This stage manifests itself in frequent infectious diseases - pharyngitis, tonsillitis, pneumonia. It is at this stage that the first rashes, especially of a fungal and viral nature, may appear. A feature in this period is that all infectious diseases respond well to treatment with standard drugs. With the diagnosis of HIV infection at this stage and timely treatment, the stage can last 10-15 years.
Progression of lymphadenopathy
Infectious diseases become persistent more severe, difficult to treat. Oral candidiasis often occurs at this stage, respiratory tract, herpes lesions of the genital organs, that is, those diseases that are extremely rare in people with a healthy immune system. There is a loss of body weight, diarrhea often occurs, which is not stopped by medication and lasts more than one month. Rashes at this stage also become generalized.
terminal stage
Transition to the stage of AIDS. Continues weight loss, turning into cachexia, diarrhea, pneumonia, skin diseases. There are so-called AIDS-associated diseases - Kaposi's sarcoma, pneumocystis pneumonia, fungal infections of the respiratory tract, nervous system. The lesions are irreversible, any treatment fails, and the patient dies after a few months.
The duration of the stages may differ from the average figures and depends on the lifestyle of the patient, the state of his immunity. Early treatment can significantly delay the stage of AIDS, and early diagnosis plays a big role in this.
Associated HIV symptoms
When it enters the body, the virus infects the cells of the immune system (T-lymphocytes), which leads to disruption of their work, weakening of the immune system and the appearance of concomitant HIV diseases. The following symptoms make it possible to suspect that a person has HIV infection:
![]()
- Fungal diseases, especially if they appear in atypical healthy person organs, for example, pneumocystis pneumonia, candidiasis of the genitourinary tract. Cryptococcosis - a fungal infection of the brain is an essential sign of HIV infection. This group also includes fungal infections of the skin.
- Frequent viral infections- for example, herpes simplex and herpes zoster with a frequency of occurrence more than once every six months, especially if it is localized on the genitals or in the oral cavity.
- Malignant diseases Kaposi's sarcoma occupies a special place among them and is an important symptom of HIV infection.
- Bacterial infections- extrapulmonary tuberculosis, secondary lesions in herpes and candidiasis (usually streptococcal).
HIV diagnosis
To date, there are several consistent methods for diagnosing HIV.
Enzyme immunoassay (ELISA)- is original and standard. Allows you to detect the presence of antibodies to the virus in the blood, has a high reliability (up to 99%). For its implementation, blood is taken from a vein and sent to the laboratory in a special test tube, the result is determined on average in a week. There may be the following options:
- negative result– no antibodies to HIV were detected (therefore, there is no infection with the virus).
- false negative result- obtained in the early stages (up to 2-3 weeks, when antibodies to HIV have not yet developed), at the stage of AIDS (when immune cells are unable to produce antibodies to infection), with errors in the diagnostic technique.
- false positive result- antibodies to HIV are present, sometimes obtained with errors in the diagnostic technique or with certain diseases and conditions (for example, alcoholic liver damage, pregnancy, condition after vaccination).
- positive result- antibodies to HIV are present.
The last two answers require further in-depth examination.
immune blotting- used with a positive response to ELISA, carried out in the laboratory, is 98-99% reliable. It consists in applying blood to a specially treated strip. Depending on the pattern shown on it, the test is considered either positive or negative.
Polymerase chain reaction (PCR)- is time-consuming and expensive and is used in doubtful cases.
Express tests- are used for mass verification of the population, their reliability is inferior to the methods described above. They require mandatory rechecking by the first two methods.
What to do if a rash and signs of HIV appear?
The appearance of a rash on the body (especially widespread, affecting several areas, difficult to treat and prone to relapse) and signs of HIV (frequent infections, especially fungal and viral lesions) does not necessarily mean infection with the virus, but is often accompanying HIV symptom and requires the discovery of the cause.
With the above rashes, it is recommended to contact the laboratory or a specialized anonymous office and undergo an analysis to detect antibodies to the virus. In the Russian Federation, there is the possibility of free (HIV centers, district clinics and hospitals) and commercial (private laboratories) examinations.
The initial method for all applicants is ELISA, according to the indications (positive and false positive), the following stages are assigned (blotting, PCR), any check is carried out without disclosing information about the patient's data. If a virus is detected, the patient is given recommendations and referrals to specialists.
Summarizing the above, we can say that although today HIV infection is not completely cured, however, with its early diagnosis and timely treatment, the patient has a significant chance to live for decades. Therefore, when the signs and symptoms described in the article appear, you should immediately be examined for the presence of a virus in the blood. In no case should you let everything take its course, the later the disease is detected and therapy is started, the worse the patient's prognosis.
is the first sign of infection. However, in most cases, such manifestations go unnoticed, which contributes to the further progression of the pathology. Therefore, if such a symptom occurs, you should make sure that there is no such a terrible disease.
Few people know how a rash manifests itself with HIV infection in women and men, a photo will help you find out the answer to a similar question, and you can find them yourself. Also at the appointment, a dermatologist is able to demonstrate a photo primary symptoms rashes in HIV.
In most cases, a rash with HIV (see photo) occurs in the following forms:
The above types of rash on the body with HIV infection are diagnosed in patients most often. Each of the ailments has its own clinical features, depending on them, and the approach to the treatment of these diseases is different.
What is the rash associated with HIV infection?
Depending on the location of the rashes on the body with HIV, they are divided into two large groups: exanthema and enanthema.
Exanthema is any rash on the skin with HIV (photo), localized only on the outside and provoked by exposure to the virus. Enanthema also denotes the presence of similar elements of dermatoses, however, they are located only on the mucous membranes and are caused by various negative factors. Enanthema often appears in the early stages of immunodeficiency, but it should be understood that such a disease can develop on its own, regardless of the presence of the virus in the body.
In the photo, a rash in the acute stage of HIV on the skin is accompanied by a vivid clinical picture. In infected patients, any dermatoses are characterized by a particularly aggressive development. At the same time, they respond poorly to therapy and are accompanied by repeated relapses.
Where does the rash appear with HIV? Such questions are often of interest to patients. A doctor is able to answer them, and when this symptom appears, it is important to conduct a differential diagnosis and find out the cause of such an ailment. How long the symptoms of a rash last in the acute stage of HIV depends on the type of pathology and the therapeutic measures taken. In most cases, the elements are located on the body, but can also affect the skin of the neck and face. Often, a rash in HIV-infected people at an early stage, a photo of it is given here, is accompanied by acute manifestations. These include:
- Increase in sweat production.
- Disorder of the intestines, manifested in the form of diarrhea.
- Fever.
- Enlarged lymph nodes.

A profuse rash with HIV and the first symptoms mentioned above are not always considered as signs of an immunodeficiency state, since they are clinically similar to influenza, mononucleosis. But even with treatment, the elements begin to spread throughout the body, the patient's condition worsens. It is already worth evaluating possible infection AIDS.
How long a skin rash appears with HIV infection is difficult to say for sure, since each patient has an individual pathology. In most cases, this kind of manifestation occurs 14-56 days after the virus enters the body.
Skin rashes with HIV infection on the body (photo) caused by fungal microflora
Mycotic lesions of the skin in immunodeficiency are among the most common. This group includes several diseases that are rapidly progressing. Skin rashes with HIV are poorly eliminated even with therapy.

Fungal lesions can be observed throughout the body, not only the trunk suffers, but also the limbs, feet, hands, scalp.
Rashes on the skin with HIV infection (AIDS), a photo of which can be shown by a specialist, may be signs of the following pathological conditions:
- Rubrophytia. It appears in most cases atypically. Red skin rash with HIV (photo) often has the appearance of flat papules. Microscopic examination reveals great amount pathogens. Such a pathology clinically resembles seborrheic dermatitis, exudative erythema, keratoderma affecting the palms and feet. Often becomes the cause of the formation of paronychia, onychia.
- Candidiasis. The first sign of HIV in men is a rash, a photo of which can be found on your own. Often, immunodeficiency manifests itself in this way in the stronger sex. A similar symptom is most often observed in young people, the elements are localized, as a rule, on the genitals, the mucous membrane of the mouth, near the anus, they can often be found on the nails, in the inguinal zone. When the rash spreads over large areas, it can ulcerate, forming weeping surfaces and accompanied by pain. If candidiasis affects the esophagus, patients are concerned about pain when swallowing, difficulty eating, burning in the sternum.
- versicolor. What are the rashes with HIV in this case? Pathology is accompanied by individual spots that do not merge, they are no more than 0.5 cm in diameter, in some cases they can reach 2-3 cm. Over time, the elements turn into papules or plaques. Such a sign can occur at any stage of AIDS.
What rashes occur with HIV that are viral in nature?

Skin pathologies of a viral nature in immunodeficiency are also quite common. They can be observed at any stage of the progression of the disease. The following dermatological lesions are considered the most common:
- Lichen simplex. The doctor at the reception can show rashes with AIDS of this nature. They look like bubbles that often burst, creating painful erosions that are unwilling to heal. Such signs are observed in the anus, oral cavity, genitals, can also affect the esophagus, bronchi, pharynx, rarely - hands, shins, spinal cord, armpits.
- Shingles. Often becomes the first sign of an immunodeficiency state. Accompanied by bubbles with exudate, if damaged, painful erosions are exposed. It is difficult to say how long the rash with HIV, which has a herpetic character, lasts, sometimes it does not go into remission. Often accompanied by an increase in lymph nodes.
- Cytomegalovirus infection. It rarely affects the skin. Such a sign is an unfavorable prognosis for AIDS.
- molluscum contagiosum. Elements in this disease are localized on the face, neck, head, and can also affect the anus and genitals. They tend to merge, are accompanied by frequent relapses.
What does a pustular rash with AIDS (HIV infection) look like in women and men: photo
 Pustular lesions in immunodeficiency in most cases are caused by streptococcus or staphylococcus aureus. As a rule, patients are concerned about such ailments:
Pustular lesions in immunodeficiency in most cases are caused by streptococcus or staphylococcus aureus. As a rule, patients are concerned about such ailments:
- Impetigo. It has the appearance of multiple conflicts, which, when damaged, form yellow crusts. They are located mainly on the beard and neck.
- Folliculitis. Clinically, the elements are similar to acne. Does HIV rash itch or not? As a rule, pathology is accompanied by itching. In most cases, the upper chest, back, face are affected, and other parts of the body also suffer over time.
- Pyoderma. Reminds outwardly warts. It is located in large folds of the skin, is difficult to treat, and is prone to constant relapses.
Manifestations in violation of the work of blood vessels

What is the rash on the skin when infected with HIV (AIDS), the photo of which is shown here, if the vessels are damaged? In this case, telangiectasias, hemorrhages, erythematous spots are observed. Localization can be very diverse, in most cases the trunk suffers.
Also, patients often develop a maculopapular rash with HIV, it is not difficult to find a photo of it. It is located on the limbs, upper body, head, face. The elements do not merge with each other, a similar rash with HIV itches.
Most people infected with the immunodeficiency virus suffer from seborrheic dermatitis. It can occur in a localized and generalized form. This pathology is a common symptom of AIDS. Accompanied by significant peeling of the affected areas.
Kaposi's sarcoma
 Many AIDS-infected patients suffer from such a malignant disease as Kaposi's sarcoma. It can occur in visceral and dermal form. The latter is accompanied by damage to the skin, while the former involves internal organs in the pathological process. Often they proceed in parallel, accompanied by both external and internal signs of the disease.
Many AIDS-infected patients suffer from such a malignant disease as Kaposi's sarcoma. It can occur in visceral and dermal form. The latter is accompanied by damage to the skin, while the former involves internal organs in the pathological process. Often they proceed in parallel, accompanied by both external and internal signs of the disease.
Kaposi's sarcoma is characterized by a malignant course, it progresses rapidly and does not respond well to therapeutic measures. The rash in this case has a bright red or brown color, localized on the face, neck, genitals, oral mucosa. It can be damaged, then patients complain of soreness. Often with sarcoma, lymph nodes increase.
As a rule, the disease develops in young people in the last stages of immunodeficiency, when patients have no more than 1.5-2 years to live.
To say specifically when a rash appears on the body with HIV infection, the photo of which can be the most diverse, is quite difficult, because there are a number of dermatoses, and they can develop both in the initial and late stages of AIDS. If you have any problems of this nature, you should contact a medical institution for diagnosis and finding out the true cause of the disease.
Skin lesions in patients with HIV infection occur in 80-85% of cases. In the dynamics of HIV infection, skin lesions are recurrent in nature, with periods of exacerbations and remissions, and in advanced forms of the disease, they acquire severe variants that are not characteristic of their clinic. According to most researchers, in the early stages of the disease, there are approximately 2.5 dermatological syndromes per patient, and in the later stages, this figure rises to 3.7. Dermatitis, eczema, staphylloderma are often observed. Infectious skin lesions are associated with herpes infection and candidiasis.
Of the mycotic diseases in HIV infection, common rubrophytosis, inguinal epidermyphytosis and versicolor versicolor are of particular importance for practice. They are characterized by rapid generalization with the formation of extensive foci throughout the skin, including the scalp, face, hands, feet, persistent flow and resistance to ongoing treatment. Rubrophytosis can give unusual clinical variants such as erythema multiforme, seborrheic dermatitis, palmoplantar keratoderma. It can be represented by numerous flat papules. The formation of onychia and paronychia is regular.
Seborrheic dermatitis, which has a prevalence of only 3% in the general population, occurs in 50% of HIV-infected people. It is one of the most common non-infectious complications of HIV infection and increases in risk and severity as CD4 counts decrease. In HIV-infected seborrheic dermatitis may be complicated by yeast infection.
With multi-colored lichen, isolated spots can reach 20-30 mm. Sometimes in the area of spots of multi-colored lichen, a mild infiltration develops.
Viral skin diseases in HIV infection are common. Herpes simplex usually affects the oral cavity, genitals and perianal region and is characterized by an abundance of elements up to dissemination, frequent relapses, a tendency to erosion and ulceration, which is accompanied by pain. Unusual localizations of herpes simplex are possible (axillary cavities, hands, shins).
With herpes zoster (develops in 10-20% of HIV-infected people), vesicular rashes are located asymmetrically along the branches of the affected nerve against the background of edema and hyperemia of the skin. The contents of the vesicles are serous, serous-purulent or hemorrhagic. Merging of pustular elements and the formation of large blisters with purulent contents are possible. Rashes are often located along the trigeminal nerve.
Skin itching and rash can also be non-specific, and serve as a manifestation of hypersensitivity to drugs. In children and young people, a skin infection caused by molluscum contagiosum is found and manifests itself in the form of raised papules on the face, scalp, torso. With HIV infection, impetigo may occur, localized mainly in the paranasal, paraoral regions and tending to disseminate with a transition to the axillary, inguinal and gluteal regions.
Vulgar warts with HIV infection tend to increase and spread over the skin. They densely cover in the first place the hands, feet and face. The same can be noted in relation to genital warts, localized mainly on the genitals and perianal region. An increase in their number and size gives the patient not only discomfort, but also various complications.
Pyococcal skin lesions in HIV infection are numerous and varied. More common are folliculitis, sometimes acquiring a clinical resemblance to juvenile acne. Their appearance may be preceded by diffuse erythema. In the future, they spread along the body, capture the shoulders, hips, perineum and other areas of the skin. Attachment of itching often leads to excoriations and eczematization.
With HIV infection, molluscum contagiosum is localized mainly in the anogenital region and around the mouth, it is characterized by multiple rashes and a recurrent course.
Skin changes associated with vascular disorders often look like telangiectasias, erythematous and hemorrhagic spots. They are usually combined with other skin manifestations. The most characteristic are numerous telangiectasias densely located on the chest, sometimes forming a crescent-shaped focus from one shoulder to the other. Foci of telangiectasias of various sizes, shapes and density are determined on the auricles, palms, fingers, shins and other areas of the skin. Telangiectasias are often accompanied by erythematous spots.
If HIV infection develops in patients with psoriasis, then this dermatosis occurs with disseminated pustular rashes.
Skin pathology is due to both emerging immunodeficiency and the direct effect of HIV.
The following are the most common skin manifestations associated with HIV infection (Fisher B., Warner L., 1987):
1. Neoplastic:
Kaposi's sarcoma;
Lymphoma (usually B-cell);
Squamous cell carcinoma;
Basalioma;
Melanoma.
2. Viral infections:
Herpes simplex;
Herpes zoster;
Chicken pox;
Molluscum contagiosum;
- "hairy" leukoplakia;
Vulgar warts;
Genital warts;
Epstein-Barr virus exanthema.
3. Bacterial infections:
Abscesses;
folliculitis;
Impetigo;
Ecthyma;
cellulite;
Ulcers (pseudomonas and polymicrobial);
mycobacterial infection;
actinomycosis;
atypical syphilis;
Burnt skin syndrome.
4. Mycotic infections:
Candidiasis;
Dermatomycosis;
Pityriasis versicolor;
Cryptococcosis;
Histoplasmosis;
Sporotrichosis;
Scopulariopsidosis.
5. Mixed infections:
Viral, bacterial, fungal.
6. Protozoal infections:
Amoebiasis of the skin.
Scabies;
Norwegian scabies.
8. Vascular lesions:
Vasculitis;
Telangiectasias;
hemorrhages;
thrombocytopenic purpura;
Hyperalgesic pseudothrombophlebitic syndrome;
Marble skin.
9. Papulosquamous dermatoses:
Seborrheic dermatitis;
Psoriasis;
Pink deprive.
10. Damage to the oral mucosa:
Angular stomatitis;
Aphthosis;
Gingivitis (simple and necrotizing).
11. Hair and Nail Changes:
thinning hair;
Hypertrichosis;
Alopecia areata;
Deformation of nails;
Changing the color of nails.
12. Exacerbation of existing diseases:
Infectious (syphilis);
Inflammatory dermatoses (psoriasis).
13. Other dermatoses:
Exanthema and erythroderma;
Xerosis and ichthyosis;
Atopic dermatitis;
Trophic disorders;
Eosinophilic pustular folliculitis;
Papular and lichenoid rashes;
granuloma annulare;
Medication toxidermia;
Itching;
Pyoderma gangrenosum;
Localized acantholytic dyskeratosis;
bullous penfigoid;
Erythema elevatum et diutinum;
Hives;
Premature aging of the skin.
The development of skin lesions of the first two groups is due to severe immunosuppression, the pathogenesis of the third is possibly associated with the direct effect of HIV on the skin. It has been established, in particular, that in the skin, HIV infects not only T-lymphocytes-helpers, but also Langerhans cells, which play an important role in dermal immune responses and, possibly, are the site of the primary introduction and accumulation of HIV in the skin.
Cosmetic defects that occur during HIV infection or its treatment often do not pose any health hazard, but cause additional suffering to patients. Examples include yellowing of the nails and straightening of the hair, lengthening of the eyelashes and bluing of the nails with zidovudine treatment, and yellow-orange skin coloration with clofazimine treatment.
Damage to the skin and mucous membranes in people infected with HIV is characterized by the fact that the usual neoplastic and infectious (mostly viral and fungal) diseases acquire a number of features: they occur in unusual age groups, have a severe course, manifest themselves atypically, poorly amenable to therapy. The nature of these changes in the skin and mucous membranes depends on the stage of HIV infection, its clinical forms, the biological properties of pathogens of secondary infections, and the severity of immunosuppression. The following diseases have the greatest diagnostic value in HIV infection: Kaposi's sarcoma, candidiasis (persistent candidiasis of the mucous membrane of the oral cavity and perianal region), simple and herpes zoster, seborrheic dermatitis, molluscum contagiosum, "hairy" leukoplakia of the oral cavity, vulgar warts. The severe course of all the above dermatoses, their generalization in the presence of general symptoms (fever, weakness, diarrhea, weight loss, etc.) are poor prognostic signs and indicate the development of clinically advanced AIDS.
Kaposi's sarcoma. A particularly severe clinical form of HIV infection is malignant neoplasms, the frequency of which is approximately 40%, which significantly exceeds their frequency in other primary and secondary immunodeficiencies. Kaposi's sarcoma is the most common malignant neoplasm.
With HIV infection, Kaposi's sarcoma is a slightly different clinical form compared to that described in 1897 by the Hungarian veterinarian M. Kaposi. Three features characterize Kaposi's sarcoma, which is not associated with AIDS - it affects men over 60 years of age; quite frequent cases of its detection among young African Negroes; the development of the disease in individuals with exogenously caused immune suppression. Regarding the origin of Kaposi's sarcoma, the most common is the opinion of a multifactorial cause of its occurrence, including infectious, genetic and environmental factors.
In patients with HIV infection, Kaposi's sarcoma is malignant and differs from its classic version. Home hallmark visceral type of Kaposi's sarcoma in AIDS is its generalized nature with damage to the lymph nodes, mucous membranes and internal organs. The skin and visible mucous membranes are involved secondarily. External manifestations are few at first and are localized mainly in the oral cavity, especially on the hard palate and in the genital area. These are juicy, cherry-colored papules, the surface of which is covered with well-defined petechiae and telangiectasias. These rashes, which are easily accessible not only for visual examination, but also for biopsy, play a decisive role in the creation of a diagnostic program. Over time, the external manifestations of visceral Kaposi's sarcoma, spreading through the skin, can become generalized.
In the dermal type of Kaposi's sarcoma, the skin and mucous membranes are primarily affected. Initial manifestations, in contrast to classical Kaposi's sarcoma, often occur on the upper body, head, neck and other areas of the skin, as well as on visible mucous membranes. In the future, the process acquires an aggressive course with spread over the skin, the formation of massive conglomerates and the involvement of internal organs. At a certain stage, the difference between the visceral and dermal types is erased.
Chemotherapy and radiation therapy for HIV infection are ineffective due to the pronounced malignant nature of the tumor, so it is not advisable to use them in order to avoid even greater suppression of immunity.
Lymphoma is the second most common tumor in patients with HIV infection. It occurs in 3-4% of cases of HIV infection. Approximately 12-16% of people with HIV infection die from lymphoma. Unlike Kaposi's sarcoma, lymphoma is not associated with any risk group.
The HIV pandemic has raised the problem of tuberculosis to the level of actuality, because tuberculosis has increased sharply among HIV-infected people aged 25-49, and the area of tuberculosis distribution coincided with the incidence of HIV infection. In the United States, where the incidence of tuberculosis until 1985 was declining at a rate of 6% per year, against the background of the HIV epidemic in 1985-1992. the incidence began to grow at a rate of 3% per year. The incidence of tuberculosis in patients with HIV infection is 2.5-15% per year, which is 50 times higher than in the general population. Moreover, as a superinfection, tuberculosis develops in the early phases of the disease with relatively high rates of CD4+ cells.
Thus, tuberculosis is returning as a major public health problem in developed countries while maintaining a high prevalence in developing countries.
Peculiarities of infection and disease in children. Children make up a small proportion of people with HIV infection. HIV infection in children can be associated with illness of mothers, transfusion of infected blood in hemophilia, low-quality infections, and drug addiction. The transmission of HIV from infected mothers can be observed in 25-30% of offspring. Childbirth in HIV-infected people obviously contributes to a more rapid development of the disease. Pregnancy favors the development of HIV infection, as it is usually accompanied by immunosuppression.
Infection of children occurs mainly in the uterus, birth canal and after childbirth. HIV is able to cross the placenta. Studies show that the fetus can be infected with HIV as early as the 8-12th week of pregnancy. Infection may also be associated with breastfeeding, since the virus is isolated from the milk of infected mothers. According to the agency Associated Press(USA), the risk of infection of a child through mother's milk is 10% with prolonged breastfeeding.
Cases are described when infected mothers gave birth to twins, of which only one was infected.
Factors influencing the risk of vertical transmission of HIV have been identified. First, it is the state of health of the mother. The higher the level of the virus in the mother's blood or vaginal secretions and the lower her immune status, the higher the risk of transmitting the virus to the child. The living conditions of the mother also play a role - nutrition, rest, vitamins, etc. It is characteristic that the average statistical risk of having a child with HIV in the industrialized countries of Europe and the USA is approximately half that in the third world countries. Having previous pregnancies increases the risk of infection. Both premature and postterm babies are more likely to be infected. The presence of ulcers and cracks in the vaginal mucosa increases the risk of having a child with HIV.
Children infected from their mothers begin to get sick 4-6 months after infection, and most of them usually die within 2 years. In children, the duration of the latent period is less than in adults (more often it lasts not for years, but for months).
In Russia, HIV infection in children has been registered as a nosocomial disease. The tragedy in Elista, Rostov-on-Don, Volgograd largely determined the further tactics of combating blood-borne nosocomial infections in the country, therefore no nosocomial outbreaks have been recorded in Russia since 1991 (V.V. Pokrovsky, 1996).
The clinical course of HIV infection in children has its own characteristics. In children infected in utero, the disease manifests itself, as a rule, already in the first months of life, and in those infected through blood transfusions, incubation reaches several years (the average incubation period for children with perinatal HIV infection is about 12 months, for children infected during blood transfusions - 40 months).
The initial signs of HIV infection due to intrauterine infection include such characteristic symptoms as growth retardation, microcephaly ("boxer's brain"), flattening of the nose, moderate strabismus, lack of weight gain, chronic diarrhea, bacterial infections. The disease proceeds more favorably in children infected over the age of 1 year. It takes 5-7 years for them to develop AIDS. The clinic of the disease also differs from adults - pneumocystic pneumonia is less common, it is replaced by lymphoid interstitial pneumonia, often proceeding as benign. These children are also characterized by secondary infectious diseases (candidiasis stomatitis and esophagitis, skin infections). Frequent signs of congenital and acquired HIV infection in children are persistent generalized lymphadenopathy, hematosplenomegaly, fever, diarrhea, psychomotor retardation, and thrombocytopenia with hemorrhagic manifestations. CNS involvement is a permanent syndrome in the clinic of HIV infection in children. The first symptoms in the form of asthenoneurotic and cerebroasthenic syndromes are diagnosed at the very beginning of the disease. In the late stages of HIV infection in children, traditional neurological symptoms are replaced by a specific CNS lesion caused by the HIV virus in the form of encephalopathies and encephalitis. These diseases lead to irreversible consequences and are often the cause of death.
A feature of HIV infection in children is also the presence of progressive lymphopenia. Almost every child suffers from bacterial, viral and fungal infections.
The most important immunological feature of children with HIV infection is the presence in the blood of exclusively high content immunoglobulins and at the same time the inability to produce antibodies when injected with antigens that cause the formation of antibodies under normal conditions.
There are almost no cases of Kaposi's sarcoma in children.
Thus, if HIV infection occurs during the neonatal period as a result of infection through the placenta or blood transfusion, then the prognosis for these children is extremely unfavorable - they should expect a progressive development of the disease, especially with CNS damage, caused directly by HIV.